The BMI Isn’t as Helpful as You Think — Especially if You’re Not A White Man
If you’ve ever been to the doctor, you’ve had your BMI (body mass index) recorded. Even if your physician didn’t specifically ask for it, all they need is your height and weight to determine if you’re within the recommended weight range.
But while we routinely rely on BMI as an indicator of health, a growing body of research is revealing that this so-called scientific measurement is causing some major medical inequities.
What is BMI?
The BMI equation, weight in kilograms divided by height in meters squared, was created in 1832 by Belgian mathematician Adolphe Quetelet. He was interested in finding a statistical relationship between body type and antisocial tendencies, believing men who diverged from the ideal (aka average) were more susceptible to criminality and other immoral traits.
This eugenic way of thought has since been disproved countless times over, but during his heyday, Quetelet’s work earned him recognition as a “father of the social sciences.” However, in hindsight, there was one glaring issue in Quetelet’s methods.
He only measured men, and nearly all of the men he surveyed were European. So his ideal man was really the ideal white man.
Also, Quetelet gathered this data in search of a moral statistic, not a medical one. The BMI’s current purpose has thus strayed very far from its originally intended purpose, and people—especially people of color—are suffering because of it.
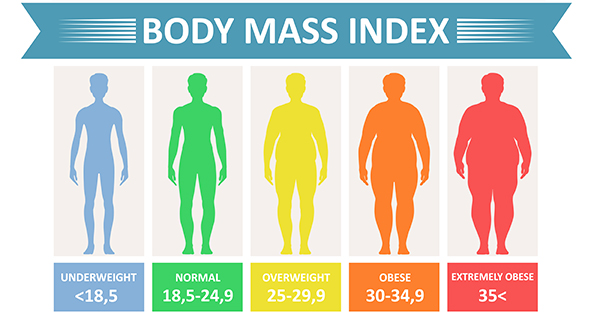
Image: CDC
How is BMI used today?
As physicians linked more cardiovascular diseases to weight in the 1950s, the medical field started to adopt the Quetelet Index—renamed BMI by physiologist Ancel Keys in 1972—as its main indicator of obesity. “When there became an increasing concern over obesity’s relation to health risks, there needed to be a basic measurement to determine who was overweight,” explains Dr. Chisom Ikeji, an internal medicine physician. “Medical professionals, insurance companies, and researchers all became okay with using BMI, not really taking into consideration how it works and how it could potentially impact health on an individual level.”
Since BMI became a staple measurement in the US and abroad, research has linked an overweight or obese BMI to an increased risk of type-2 diabetes, cancer, heart disease, and other serious conditions. Currently, the CDC and World Health Organization define a BMI between 18.5-24.9 as healthy. A BMI below 18.5 is underweight; a BMI between 25-30 is overweight; and a BMI over 30 is obese.
While the CDC notes that BMI is “not diagnostic of the body fatness or health of an individual,” Dr. Ikeji says some physicians treat it as so. “If physicians are looking at that number without looking at the patient, or considering how their body composition might affect the BMI, they’re going to make an assumption about a patient,” she continues. “That’s a general bias all health professionals have.”
That bias doesn’t start in the waiting room either. For decades, health insurers routinely denied people coverage or charged them excessive premiums based solely on their BMI. The Affordable Care Act (ACA) has since banned discrimination against preexisting conditions, including severe obesity, for newly purchased insurance plans. However, the ACA still allowed workplaces to penalize employees up to 30% of the total cost of their coverage if they didn’t satisfy the requirements of a health-contingent wellness program.
This loophole was closed in 2019 after the AARP sued the Equal Employment Opportunity Commission, arguing that some of these programs’ required biometric screenings (which could include BMI and waist measurements) invaded employees’ privacy.
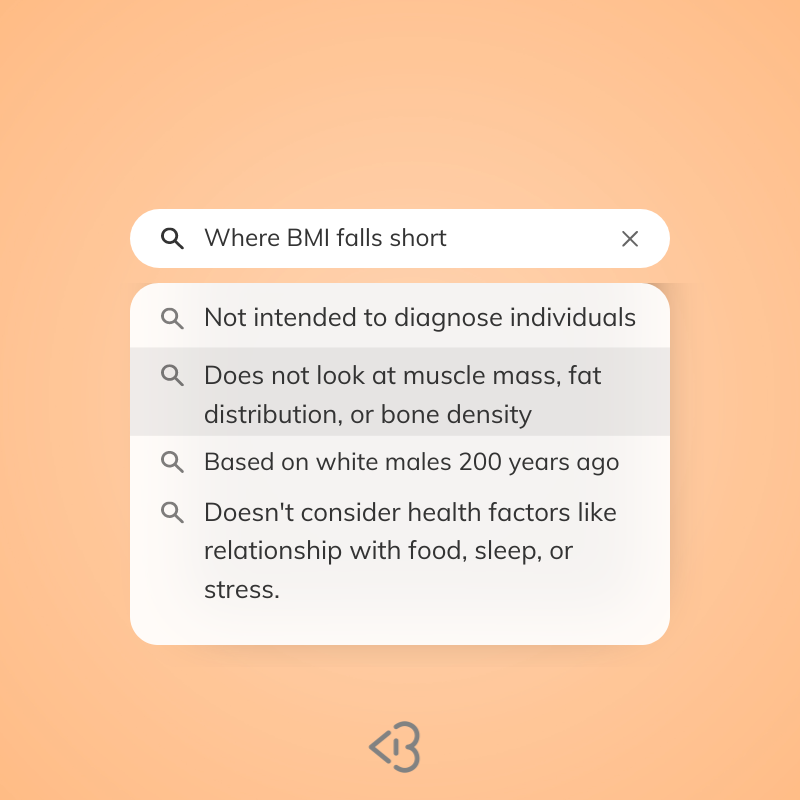
Where does BMI fall short?
BMI became a medical standard back when approximately 13% of the US population identified as non-white, but now that this figure has grown to over 40%, reliance on the BMI is leading to disparities in who is considered at risk for potentially life-threatening diseases. As Dr. Ikeji summarizes, the primary reason BMI doesn’t work as a blanket measure is because it doesn’t account for racial variations in body composition.
In practice, BMI is used as a proxy measurement for adipose tissue (the technical term for body fat), which increases our risk of disease when in excess amounts. However, the fat-to-weight ratio (what I’m dubbing the FWR) isn’t the same for everyone.
A 2009 study of reproductive-aged women found that at the same BMI, white women had the highest total fat mass while Black women had the lowest. (The magnitude of the discrepancy also grew as BMI increased.) A following report attributed the difference to Black women, on average, having a higher percentage of muscle and bone mass when compared to white women.
Due to this racial variation, a 2003 study found that the optimal BMI range for Black patients actually extended to 30 instead of the CDC-recommended 25, with a consistent risk to life span not observed until a BMI of 37. On the other end, Asian women tend to have a higher percentage of body fat than white women, doubling their risk for type-2 diabetes at the same BMI. Across racial lines, an estimated 74 million Americans—who either seem overweight, but really aren’t, or who seem of a healthy weight, but still have metabolic issues—have had their wellness misjudged on the basis of BMI.
@drchizikeji BMI is a scam 🥺 #blackdoctors #medicine #health
These studies (and many others that focus on different communities) demonstrate the BMI’s failure as an equitable indicator of body fat. But even if the BMI was reformulated to accurately measure adipose tissue for all women, it still wouldn’t be foolproof. That’s because even if women have the same amount of fat, how they carry it is also important.
In the 2009 study, researchers found that Hispanic and white women held most of their fat in their midsection while Black women favored their legs. And while being pear or apple-shaped usually only comes up when talking about how to dress for our silhouette, studies show that fat around one’s midsection increases one’s risk for cardiovascular disease while leg fat is actually negatively correlated with it. Factoring in both body composition and fat distribution, it becomes abundantly clear that the BMI, to put it scientifically, is not giving.
Are there any alternatives to BMI?
Even though it’s been made abundantly clear that the WHO’s BMI ranges aren’t one size fits all, countries are redefining them to better predict health risks. Japan, China, and India have all lowered the cutoff for a healthy BMI to account for the average body composition of their primarily Asian populations, while researchers in South Africa, Ethiopia, and Kenya have investigated which cut-offs best suit their demographic profiles as well.
In the UK and the US, healthcare professionals are pushing for official ethnicity-specific BMI guidelines, but there should also be reform in how physicians are taught to judge a patient’s BMI. While it would have been nice, Dr. Ikeji didn’t learn about the racial variations in BMI-related risks during medical school. “I had the privilege of my mom being a physician,” she says. “At a young age, she told me that the BMI does not make sense for us.”
Unlike Dr. Ikeji, most practicing doctors in the US don’t have a medically-trained, Black mother to provide this supplemental education (but should definitely be mandatory) education. Not every physician is going to question whether a Black woman with a BMI of 29 is actually overweight or if an Asian-American woman with a BMI of 24 is at risk for type-2 diabetes.
It shouldn’t be the burden of patients to know all of this, but until the CDC’s guidelines catch up with reality, Dr. Ikeji recommends keeping tabs on your health by minimizing processed foods and stress, making sure you can go up a few flights of stairs without getting winded, and getting routine bloodwork done every couple of years.
If you’re concerned about your weight or aren’t sure if you should be, then consult a physician and ask them to measure your waist-to-height ratio, which has proven to be a better indicator of cardiometabolic risk. And in the final, wise words of Dr. Ikeji. “If you have a provider that’s only looking at your BMI, find somebody else.”























12 thoughts on “The BMI Isn’t as Helpful as You Think — Especially if You’re Not A White Man”
There are 12 comments posted by our users.
But… how can I know what a healthy weight range is for me?
Hi Tanya,
That’s the magic question! I’m by no means a doctor so I can’t give medical advice, but here’s a summary of Dr. Ikeji’s statements from the article: If you can easily do moderately energetic activities (like going up the stairs or playing around with kids), have a clean bill of health based on routine bloodwork, and eat a balanced diet without an excess of processed ingredients, then you shouldn’t be too worried about your weight barring any other factors.
If you do have concerns, it’s best to get medical advice from a physician, but just remind them that your optimal weight might differ from the standard based on your racial background. I hope that helps!
BMI was explained to me as an average, to be able to compare, Wich for some people sounds like hell. For me it helped, it gave me a goal. Something strict that I could work towards. It was never used as something that said you were ugly. It was always used as an average where I’m from.
When I was young, I was extremely stressed about my higher BMI. I always believed that if my BMI was higher than it should be, I was obese. I always have (probably from my father) more prominent and muscular calves and heavier bones, so going by BMI data is nonsense. BMI is a scam, and it only makes people stressed.
Exactly! So many of us get stressed about it when it doesn’t even apply to us accurately. I’m so glad more people are talking about this now!
Wow, thanks for this insightful article! I’ve had a gut feeling for a while now, about how using a single scale to judge millions of patients is not the best way to go about things, but the information contained here really solidifies it. It’s crazy how something developed centuries ago for non-medicinal purposes is still widely used today. I’m glad that the faults in the BMI system are being brought to light now. Hopefully, professionals can come up with new methods that don’t generalize and exclude other ethnicities/races, like the waist-to-height ratio Dr. Ikeji mentioned.
Just a little note on ethnicity, it might be helpful to specify which part of Asia you’re referring to when you say “Asian Americans” or Asian people (i.e east asia, south asia, etc), as Asia is a massive continent with a vast quantity of skin tones/cultures and body types as well (I am also asian-american!)
Hi Elena! Yes it’s wild that we still treat the BMI as a dependable indicator of health and wellness. As for the comment on ethnicity, you’re totally right that there’s so much diversity within the term Asian that it sometimes feels like an overgeneralization to use it. In the research I found, a lower BMI was ideal for both East Asian and South Asian populations so I decided to use the broader term since the recommendation seemed to apply overall, but I’m sure there are nuances for specific communities because of the same reason you’re pointing this out. Thanks for being so intentional with your feedback and I’ll keep this in mind the next time I write something referencing diasporic communities!
Thanks for taking the time to read my comment and taking kindly to the feedback! And I just wanted to add, the fact that Quetelet wanted to compare body-type (or looks in general) and criminality is so bizarre. It’s pretty well known that looks have got nothing to do with whether you’re a good person or not (like Ted Bundy, Richard Ramirez, etc). Even if this wasn’t a widely accepted sentiment in the 1800s (which I kind of doubt), there shouldn’t be any excuses for current medical professionals to be using the BMI system.
I do not mean this to be rude in any way. But how is saying asian an overgeneralization but European isn’t?
Oh, you’re probably right. I only mentioned the “Asian” part because I myself am asian. However, I do understand that there are a wealth of different cultures and countries in Europe, I’m just not super educated about them yet. And that goes for every continent as well
It’s definitely not the best but it’s used as an average from where I’m from. I don’t know how it is in America but here it’s not used to tell if your healthy or not. It was also common knowledge that you could even seem bigger even though you’re perfectly in the middle. It was an average. Something to compare yourself to. It isn’t used here as a precise scale
Hi! It’s not used purely diagnostic here either, but I think it’s a bigger issue when physicians use it as an indicator of health without taking into account how there are different ideal BMI ranges for different communities. I think it’s also an issue when you have a normal BMI but have some other underlying health factors. Like, personally, I’ve always been at a recommended BMI but I didn’t find out until I got some bloodwork done that my cholesterol was very high for my age. I think if I presented as overweight, then that would have been discovered sooner, but you never know for sure.